In 2015, Oneview put video cameras above patient televisions in a US hospital. The technology itself was not new, but the use of video calls in healthcare were a rarity. While the idea of remote connectivity into the patient room was enticing, especially for a healthcare system where clinicians worked across campuses, adoption was slow. Clinicians wanted to see patients, and patients expected to see clinicians, not on a screen, but face-to-face at the bedside.
Fast-forward to 2020 and as the pandemic took grip, video became a necessity. The ability to communicate with hospital patients without entering the room enabled the preservation of scarce PPE. In desperation, healthcare systems deployed every manner of solution, from baby monitors to home video cameras. We were privileged to be able to support our customers by deploying video communication services on Oneview tablets at the bedside.
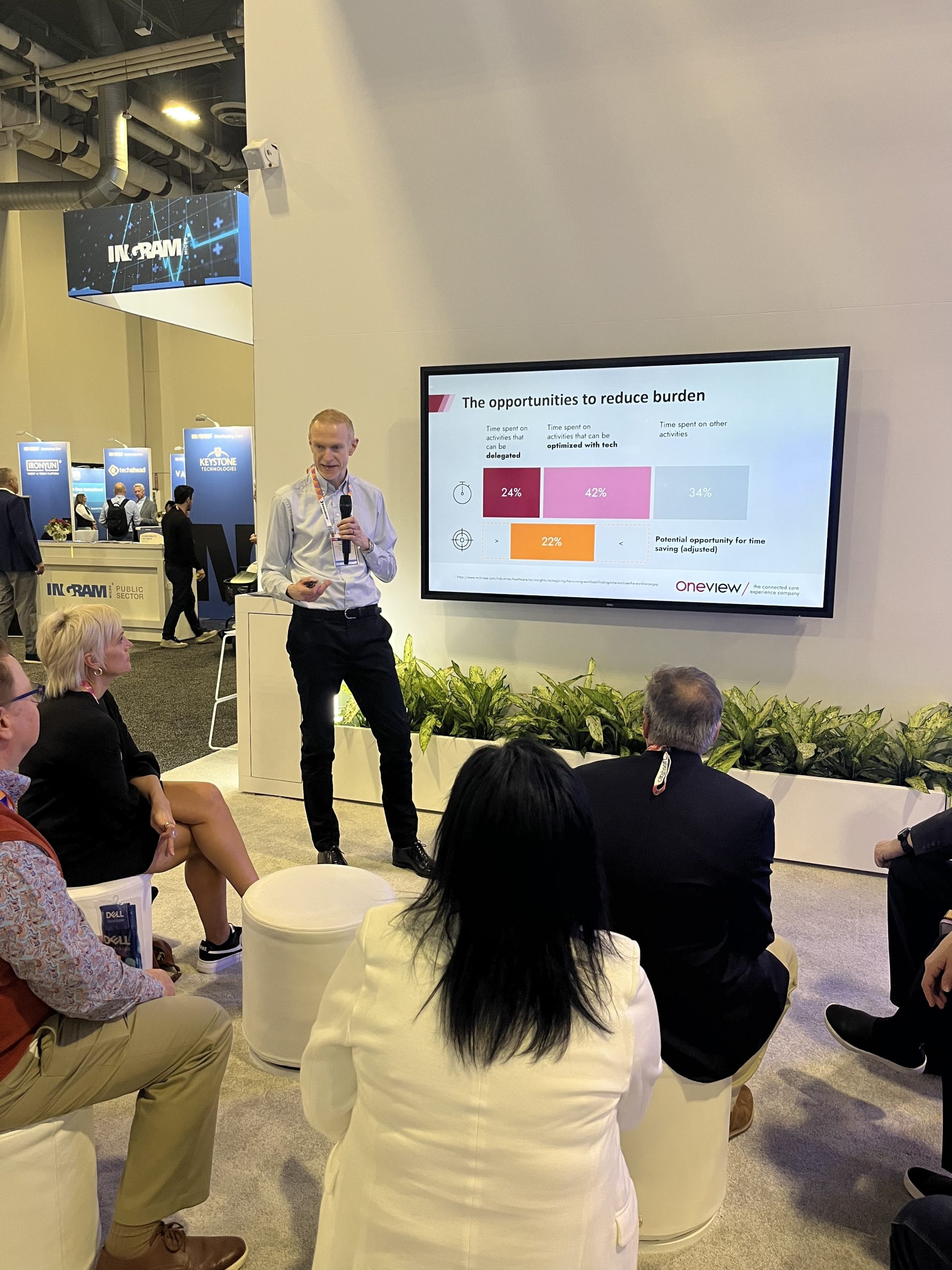
Emerging from those dark days, the use of video in healthcare was no longer a rarity. In every aspect of our life, video had been the key to connection and to sustaining relationships. Healthcare systems stepped back and considered how technology that had been deployed tactically, might be used strategically to alleviate the post-pandemic staffing crisis. With contract staff hours relative to permanent staff hours up 91% from March 2020 to March 2023, and projected gap of between 200,000 and 450,000 nurses available for direct patient care by 2025, new care models enabled by technology are key to financial sustainability. These models, combining on-floor nurses with virtual colleagues, promise a better care experience for nurses as well as for patients.
With the ability to video call reliably and securely into the patient room, virtual nurses can support their on-floor colleagues, taking on non-physical care needs such as admission interviews, patient education and discharge preparation. By off-loading these aspects of patient care, on-floor nurses can focus on physical care and nurturing care that requires face-to-face contact. And in a world of nurse burnout stress, every little bit helps.
Supporting this post-pandemic care model innovation is a key part of Oneview’s strategy. We’ve heard from our customers that organizations don’t want to be forced to adopt proprietary solutions, or solutions that lock them in. Now, we’re excited to announce the release of our Virtual Care API, bringing interoperable virtual care to the hospital room and the patient’s television. The Virtual Care API enables customers to choose the best solution for their needs – at an enterprise-level, a facility-level, or even a unit-level. Our certification program ensures that customers can select a vendor that is proven with the Virtual Care API. We are pleased to announce that Caregility is the first vendor certified, with more vendor certifications in progress.
It’s taken nearly a decade, but the days of video cameras becoming an integral part of great inpatient care are finally upon us.
Health System Workforce Market & Solutions: Flash Intelligence | Kaufman Hall. www.kaufmanhall.com. Published May 23, 2023. Accessed November 8, 2023. https://www.kaufmanhall.com/insights/research-report/health-system-workforce-market-solutions-flash-intelligence
Berlin G, Lapointe M, Murphy M, Wexler J. Assessing the lingering impact of COVID-19 on the nursing workforce | McKinsey. www.mckinsey.com. Published May 11, 2022. https://www.mckinsey.com/industries/healthcare/our-insights/assessing-the-lingering-impact-of-covid-19-on-the-nursing-workforce